
Using SPICT-LIS
Why use the SPICT-LIS?
SPICT-LIS helps identify people with one or more general indicators of poor or deteriorating health and signs of life shortening conditions for a palliative care review and future care planning.
We offer these people the best available, appropriate treatment integrated with holistic palliative care. SPICT-LIS looks for changes in health, burden of illness and the needs of people and families.
Early identification for palliative care avoids harm and improves treatment and care.
Using SPICT-LIS to review holistic care needs and plan care.
Poorly controlled symptoms: Give the best available, appropriate treatments for underlying conditions, stop medicines/tests not of benefit; use effective palliative symptom management.
Depends on others more due to deteriorating functional ability, physical frailty and/or mental health problems. Look at options for more care and support for the person and their family.
Hospital admission, more clinic visits or a decline in health: Review current care, treatment and medication. Discuss available options if health worsens. Acknowledge uncertainty.
Holistic care needs (physical, emotional, social, spiritual) that are difficult to manage. Consider specialist palliative care review or involve another appropriate specialist or service, if available.
Coordinated care at home: Plan care and support from the primary care team and/or other community services or workers. Involve the local community. Support family carers.
Decision-making capacity. Plan ahead if this will get worse. Record details of close family/friends and any legal proxies. Involve them in decision-making if capacity is impaired.
Future care plan: Agree, record, share and plan to review. Include plans for urgent/emergency care and treatment if the person’s health (or care at home) deteriorates rapidly or unexpectedly.
Taling about future care planning.
Future care planning discussions may include:
• What matters for this person if their health changes.
• Benefits, harms and costs of hospital admission, outpatient visits, tests and treatments (e.g., IV antibiotics/fluids; surgery; cancer treatments, treatments for heart or kidney disease; tube feeding; oxygen or ventilation.
• Treatments/medicines that help, could stop, will not work or have a poor outcome.
• Cardiopulmonary resuscitation (if relevant).
• Choosing legal proxy decision-makers.
• Help and support for family/friends/carers.
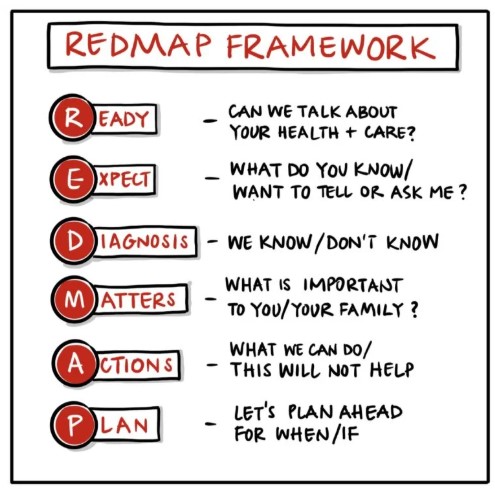
Tips on starting conversations about care planning.
-
- I wish we had a treatment for…, but could we talk about what we can do if that’s not possible?
- I am glad you feel better and I hope you will stay well, but I am worried that you could get ill with…
- Can we talk about how we might manage when we are not sure what will happen or when?
- If you get less well, what is important for you? What would (name) say about this? Why is that?
- Some people find it helps to talk about whether to go to hospital or not if they get ill…
www.spict.org.uk
January 2025