
UK resources for professionals
- General Medical Council
Treatment and care towards the end of life: good practice in decision making
Decision making and consent (2020) - Royal College of General Practitioners, London
Palliative and end of life care toolkit
Daffodil standards for advanced serious illness and end of life care (RCGP and Marie Curie) - Royal College of Physicians, London
End of life care in the acute setting (2021)
Talking about dying (2018) - Royal College of Physicians and Surgeons of Glasgow
Using RED-MAP (RED-MAP model for conversations about future care planning)
REDMAP Framework (2021) - National Institute for Health and Care Excellence (NICE)
End of life care for adults – service delivery (2019)
Care of dying adults in the last days of life (2015)
End of life care for infants, children and young people with life-limiting conditions: planning and management (2016)
- Scottish Government:
Strategic framework for action on palliative and end-of-life care (2015) (Recommends SPICTTM )
Do not attempt cardiopulmonary resuscitation (DNACPR) – integrated adult policy - Healthcare Improvement Scotland (ihub)
Anticipatory care planning – toolkit (updated 2021) - NHS Education for Scotland
Palliative Care Portal (includes link to Scottish Palliative Care Guidelines)
Resources for Professionals on Bereavement – Support Around Death
- UK Association for Palliative Medicine
- Hospice UK
- Scottish Partnership for Palliative Care
- Cecily Saunders Institute of Palliative Care, London
Palliative care outcome scale (POS) - Gold Standards Framework
- ReSPECT (Recommended Summary Plan for Emergency Care and Treatment)
- British Medical Association
End-of-life care and physician-assisted dying (2016; volume 1:part 4, page 57 – identification)
- Good life, Good Death, Good Grief Resources for the public, patients, families and professionals (Scotland)
- Dying Matters Resources for the public, patients, families and professionals (UK)
- Early Palliative Care (Video resources for professionals, patients and families)
International palliative care resources for professionals
- World Health Association – palliative care
Integrated, people-centred palliative care - International Association for Hospice and Palliative Care
- Worldwide Hospice and Palliative Care Alliance
Palliative care toolkits
- European Association for Palliative Care
International Consensus on Advance Care Planning (Lancet Oncology, 2017); EAPC blog update
EAPC primary palliative care group – Resources for development of palliative care in the community: Toolkit + Poster
- Palliative Care Australia
CareSearch – palliative care knowledge network
The ADVANCE project – national education programme on advance care planning in primary care
End of life care essentials for acute hospitals
Palliative Care Phase tool
End of Life Directions for Aged Care (ELDAC)
- Center to Advance Palliative Care (CAPC, USA)
Talking about future care – resources on advance/ anticipatory care planning
- REDMAP framework Communication with patients and families about deteriorating health and future care planning
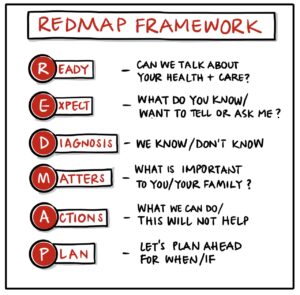
Using REDMAP video: Royal College of Physicians and Surgeons of Glasgow
ACP-TALK video: Staying in my Care Home or Going to Hospital (Pre-Covid)
ACP-TALK video: Care in the Last Days of Life (Pre-Covid)
- PREPARE for your care (USA) – public information and resources to support advance care planning)
- Think Ahead (Planning for death & dying) (Ireland) – Resources and advice for the public and professionals from the Irish Hospice Foundation
- The ADVANCE project – national education programme on advance care planning in primary care
- The Conversation Project (USA)
- Respecting Choices Advance Care Planning Programme (USA)
- Serious Illness Care Program (USA) – Resources and training in talking about serious illness
- Vital Talk (USA) – Clinical communication resources and training
- Stanford Letter Project (USA)
- CLEAR Conversations Project (USA)
- Let’s talk about death and dying (UK)- booklet and video resources for patients and families from Age UK
- Best Case/ Worst Case Communication Tool (USA) – Structured approached based on a graphic decision-aid to support difficult conversations about high risk surgical interventions with people whose outcomes are likely to be poor.
Shared Decision-Making
NHS Scotland – Realising Realistic Medicine, 2017
NHS Education for Scotland – Having realistic conversations (DECIDE model)
NHS England – Resources on shared decision-making
Choosing Wisely UK – questions to ask your doctor or nurse about tests and treatments
National Institute for Clinical Excellence (NICE), UK – Shared decision-making
Cochrane UK – Sharing health evidence
Mayo Clinic, USA – Shared Decision Making National Resources Center
Ottawa Hospital Research Institute, Canada – patient decision aids
Communication and patient experiences – references and resources
Leaflet for patients and families: What happens when someone is dying.
Kimbell B, Murray SA, Macpherson S, Boyd KJ. Embracing inherent uncertainty in advanced illness. BMJ 2016; 354 doi: https://doi.org/10.1136/bmj.i3802
– Jacobsen J, Brenner K, Greer JA, Jacobo M, Rosenberg L, Nipp RD, Jackson VA. When a patient is reluctant to talk about tt: A Dual Framework to focus on living well and tolerate the possibility of dying. J Palliat Med. 2018 Mar;21(3):322-327. doi: 10.1089/jpm.2017.0109. Epub 2017 Oct 3. PMID: 28972862.
– Jackson VA, Jacobsen J, Greer JA et al. The cultivation of prognostic awareness through the provision of early palliative care in the ambulatory setting: a communication guide. Journal of Palliative Medicine. 2013; 16(8):1-7.
– Bernacki R, Hutchings M, Vick J, et al. Development of the Serious Illness Care Program: a randomised controlled trial of a palliative care communication intervention. BMJ Open 2015;5:e009032. doi:10.1136/bmjopen-2015009032
– Bernacki RE, Block SD. Communication about serious illness care goals: a review and synthesis of best practice. JAMA Int Med 2014;174:1994-2003.
– Pino M, Parry R, Land V, Faull C, Feathers L, Seymour J. Engaging Terminally Ill Patients in End of Life Talk: How Experienced Palliative Medicine Doctors Navigate the Dilemma of Promoting Discussions about Dying. PLoS ONE 2016; 11(5): e0156174. doi:10.1371/journal.pone.0156174
– Parry R, Land V, Seymour J. How to communicate with patients about future illness progression and end of life care: a systematic review. BMJ Supportive Palliative Care 2014; doi:10.1136bmjspcare-2214-000649.
Smith AK, White DB, Arnold RM. Uncertainty, the other side of prognosis. N Eng J Med 2013;368:2448-2450.
Kendall M, Carduff E, Lloyd A, et al. Different Experiences and Goals in Different Advanced Diseases: Comparing Serial Interviews with Patients with Cancer, Organ Failure or Frailty and Their Family and Professional Carers. J Pain Symptom Management 2015; http://dx.doi.org/10.1016/j.jpainsymman.2015.02.017
California Health Foundation. Gather Round: Understanding How Culture Frames End-of-Life
Choices for Patients and Families. 2014
Milford Care Centre: Compassionate Communities. Let’s talk about illness, death and dying
(Videos for patients, families and professionals: public awareness projects)
